Featured in MyeNews, Spring Issue, 2015.
John Fullagar gave the consumers perspective at the recent DC Down Under Symposium
DC Down Under is an annual symposium organised by the Dendritic Cell Research group (of the ANZAC Research Institute) and has attracted a serious scientific following since it began. The Symposium showcases cutting edge dendritic cell (DC) immunology research and its clinical application. It provides an opportunity for young investigators and established leaders in the field to present their work in a professional yet intimate environment, ultimately, providing us with a selection of scientific presentations of the highest calibre.
DCR maintains active consumer involvement in their research. They have a DCR Consumer Committee, consisting of individuals who either have cancer, are in remission or who are carers of cancer patients, that meets bi-annually. The committee functions assist with reviewing research proposals; informing study design, and guiding development of various forms of media for general community distribution.
For the first time this year, consumers on this panel were invited to attend and present at this Symposium giving researchers the opportunity to communicate their work with consumers, and enabling consumers to communicate how having their condition impacts their lives.
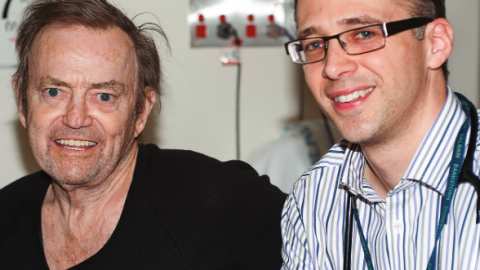
John Fullagar was invited to present at this year’s DC Down Under Symposium held on 6-7 August at the Sydney Medical Education Centre in Concord. John, now 73, has spent his career as a professional engineer and manager. Now retired from paid work, he’s a serial volunteer, including a position as Secretary of the North Shore Prostate Cancer Support Group. John shares his story which was presented at the Symposium, below.
John’s Journey…
My multiple myeloma is the second of three personal cancer journeys – for prostate (2002), then myeloma and now a basal cell carcinoma (2015). The myeloma journey began in March 2007. For decades, I had suffered respiratory irritations, so my GP (Dr Elaine Wilson,) referred me to a physician specialising in diagnosis and pathology (Dr Karl Baumgart). Some 6 months later, after a battery of allergy and other tests, Dr Baumgart revealed I had a “monoclonal gammopathy of uncertain significance” (menacing words to a medical layman) which he said “we need to keep an eye on” adding that “there’s a 20 % chance it will become myeloma within 20 years” (even more anguishing!)
He was right, of course. His regular testing from 2007 to 2010 led to suspicion of myeloma (March 2010) and my referral to Haematology at Royal North Shore Hospital, with the suggestion that bisphosphanates may strengthen my bones.
A man can be fortunate. I was born and nurtured by healthy intelligent parents, Margaret (my wife) is caring and patient and I have three doctors who have provided first-class medical treatment for my journey and have shown whole-of-person care: Dr Elaine Wilson (GP), Dr Karl Baumgart (specialist physician) and Dr Matthew Greenwood (my RNSH haematologist). And others have also excelled: the friendly and gentle “vampires” of PaLMS, who have regularly extracted my blood for tests, and Debbie Taylor, physiotherapist at RNSH.
After confirmation of my disease, Dr Greenwood started me on bisphosphanates (Zometa), as Dr Baumgart had suggested, and prescribed two cocktails of chemotherapy (one after the other) to evaluate each cocktail’s effect on my disease:
- CAD (Cyclophosphamide, Adriamycin & Dexamethosone) was administered as four infusions at 4-weekly intervals but its effect was considered “inadequate”
- CTD (Cyclophosphamide, Thalidomide & Dexamethosone) was taken in three 3-week cycles and performed better, so the Hospital’s stem-cell transplant team agreed to let me into their program.
Then followed preparations for harvesting my stem cells, which meant giving myself daily injections (a huge hurdle for me, given my paranoia about any needle getting closer than 6 feet). Zometa was also suspended (mid Sept) and the harvest (using aphoresis) was in October.
Next came the big 3-week hospital stay – in isolation conditions to prevent infection. First I had a sledge-hammer dose of chemo, followed the next day by re-infusion of half the stem cells harvested weeks earlier. (The other “half” is still in frozen storage in case it is needed later.) Dr Greenwood says I had a hard time in hospital. I remember the isolation constraints (particularly on visitors) and the scale-like skin eruptions around the Picc line and cannulas that were used for infusions during my stay. Some residue of that scale is still evident five years later.
A month after the transplant, Zometa was started again (until mid-2012). Then three months after the transplant, I started 12 months of Thalidomide at 50 mg per day with encouraging results. Since then, no test results have been anywhere near 1000 and, for a short time, my results were dropping towards “normal”. However, I was getting peripheral neuropathy (deadening of nerves at the ends/tips of my fingers and toes) which is typical with Thalidomide. As a person who loves playing the organ for church services, I found this traumatic, so we stopped the Thalidomide.
Early in 2012, Dr Greenwood asked my GP to initiate re-immunisation against the range of diseases (including those commonly encountered in childhood). These immunities had been “knocked-out” by the stem-cell transplant and associated procedures.
In the first quarter of 2012, my free Kappa resurged modestly – up to about 170 mg/l – but it jumped to over 500 in July, so (despite the potential of increased neuropathy) we decided that I should renew intimate relations with Thalidomide – starting at 100 mg/day. My free Kappa then dropped again (to the region of 100-200) so in April 2013 we reduced the Thalidomide to 50 mg/day – and stopped it completely in July, on account of my absolute misery from the neuropathy’s impact on my organ playing. Since July 2013, I have had no cancer medications at all – there’s just been regular monitoring (through blood tests at PaLMS) and consultations with Dr Greenwood.
In the year after we stopped Thalidomide, my free Kappa went for a disappointing walk-about (between 100 and 350 mg/l) but has since stayed below 170, with a consistent downwards trend, and my most recent test (in July 2015) delivered a “best-yet” result (62.3 mg/l). The “normal” level of 20 mg/l (which will allow Dr Greenwood to proclaim “complete remission”) is within sight – exciting!
That’s most of my story to date – but “there’s more”: none of this evidence points to me doing anything that might deserve such an encouraging outcome. Others have given me superb medical care but another factor has also been at work. Since diagnosis, I asked for the prayers of my own parish church and of many personal friends. I am really grateful for this support. It’s now 5 years since my transplant – and that’s already a longer survival than the median I had been led to anticipate, so let me publicly say a huge “thank-you” to God for this blessing. He has given by helping me get so well.